Navigating Pregnancy and Lactation with PCOS: What You Need to Know
Polycystic Ovary Syndrome (PCOS) affects 1 in 10 women of reproductive age, often making conception a challenging journey. However, the hurdles don’t end there. Pregnancy and lactation bring unique concerns for women with PCOS, but with the right approach to nutrition and health, they can manage these challenges effectively. Let’s dive into the most common issues women with PCOS face during pregnancy and lactation, along with practical tips for staying healthy throughout this exciting time.
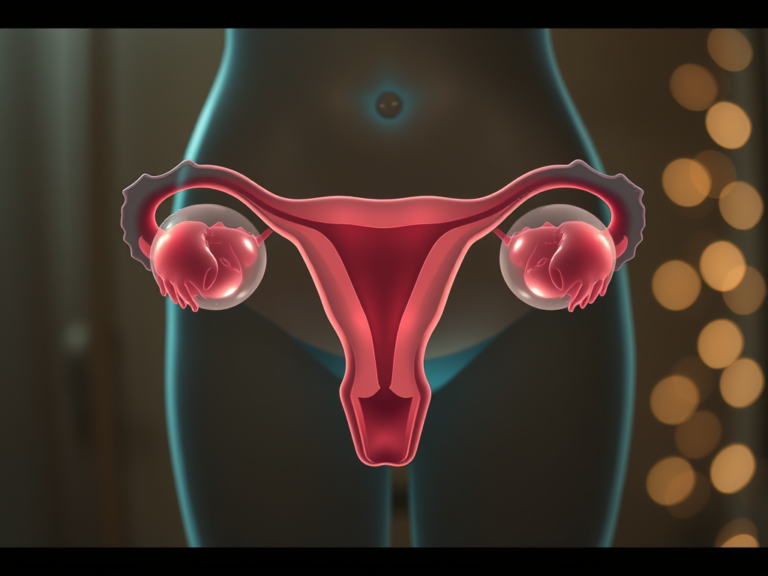
Understanding PCOS and Its Impact on Pregnancy
PCOS is characterized by hormonal imbalances, particularly excess insulin and androgens (male hormones). These imbalances make it difficult for many women to conceive naturally, often leading them to seek fertility treatments. While pregnancy brings joy and relief after the struggle to conceive, it also introduces new challenges. Women with PCOS are at a higher risk for complications such as:
- Gestational Diabetes Mellitus (GDM)
- Preeclampsia (high blood pressure during pregnancy)
- Preterm labor
- Miscarriage
This increased risk is mainly due to the insulin resistance and weight concerns common in women with PCOS, which can exacerbate issues during pregnancy. Proper medical nutrition therapy (MNT) and guidance from healthcare providers are crucial in reducing these risks.
Common Emotional Concerns for Pregnant Women with PCOS
Many women with PCOS have complicated relationships with food and body image due to the societal pressures of thinness and the common symptoms of PCOS (e.g., weight gain, excess hair growth, and male-pattern baldness). These concerns can manifest in various ways during pregnancy, such as:
- Fear of weight gain: Some women may try to restrict carbs during pregnancy, concerned about gaining too much weight or developing GDM. However, it’s essential to remember that healthy, whole grain carbohydrates are necessary for both the mother’s and baby’s health. Dietitians can help women understand the importance of balance.
- Abandoning restrictive diets: On the other hand, some women may feel that pregnancy gives them free rein to eat whatever they want, potentially leading to binge eating and excessive weight gain. Balanced meals with appropriate portions of carbs, protein, and fats are key.
Addressing emotional well-being is just as important as the physical aspects of pregnancy. Women with PCOS often benefit from extra support, whether from dietitians, mental health professionals, or support groups, to navigate these emotional hurdles.
Health Risks and Dietary Recommendations
For women with PCOS, pregnancy is often considered a state of pre-gestational diabetes. As such, adopting a diet similar to that recommended for managing GDM can help. This includes:
- Slight carbohydrate reduction (35-40% of total calories) with an emphasis on whole grains and high-fiber foods.
- Distributing carbohydrates evenly throughout the day and including protein-rich foods in all meals and snacks to stabilize blood sugar.
- Limiting simple carbs like sweetened beverages, candy, and desserts to prevent spikes in insulin.
Physical activity, such as post-meal walking, can also help manage blood sugar levels. Early screening for GDM (around 20 weeks gestation) is often recommended for women with PCOS to catch any issues early and implement proper management strategies. However, 24 weeks is the standard for all pregnant women.
Supplements During Pregnancy: Is It Safe to Take Inositol and NAC?
Many women with PCOS take supplements like inositol and N-acetylcysteine (NAC) to manage their symptoms before pregnancy. But are these safe to continue during pregnancy or while breastfeeding?
Inositol
Some studies suggest that inositol, particularly myo-inositol, can help with insulin sensitivity and even reduce the risk of GDM. Research suggests that taking 2 grams of myo-inositol twice daily can significantly improve fasting insulin and glucose levels. For women with a family history of type 2 diabetes, this supplement has been found to reduce the risk of developing gestational diabetes by a remarkable 40% compared to those who didn’t take it. In addition, it helps lower blood pressure, cholesterol, and triglycerides, while improving “good” HDL cholesterol levels. What’s more, myo-inositol has also been shown to reduce the chances of fetal macrosomia, a condition where the baby grows too large in the womb, which can lead to complications during delivery. Not only does it benefit the mother by improving her insulin response, but it also supports healthier fetal growth.
Interestingly, studies suggest that myo-inositol may work even better than traditional medications like metformin or pioglitazone in improving insulin sensitivity. Animal studies also indicate that high doses of myo-inositol can enhance the body’s ability to manage blood sugar by improving how cells respond to insulin, particularly in muscle tissue. It’s generally considered safe during pregnancy and lactation, but always consult with your healthcare provider before continuing any supplements.
NAC
N-Acetylcysteine (NAC), an antioxidant supplement often used to manage PCOS symptoms by reducing oxidative stress and improving insulin sensitivity, is generally considered safe during pregnancy when taken at recommended doses. However, breastfeeding mothers should take special precautions. If you take NAC orally, it’s recommended to pump and discard your milk for 30 hours afterward to minimize your baby’s exposure.
That said, when NAC is taken via inhalation, it’s minimally absorbed into the bloodstream, so breastfeeding can typically continue without any extra precautions. However, as with inositol, speak to your healthcare provider to ensure it’s right for you.
Is It Safe to Take Metformin While Breastfeeding?
Metformin is commonly prescribed for women with PCOS during pregnancy to help manage insulin levels and reduce complications. But is it safe to continue while breastfeeding?
Current research indicates that metformin does pass into breast milk, but only in small amounts that are unlikely to harm the baby. Several studies have found no significant impact on infants’ growth or development. However, because research is still limited, it’s essential to discuss the risks and benefits with your healthcare provider before deciding whether to continue metformin while nursing.
Breastfeeding and PCOS: Challenges and Solutions
Breastfeeding can be another challenging area for women with PCOS due to hormonal imbalances affecting milk production. Some women may have difficulty producing an adequate milk supply because their breast tissue doesn’t undergo the necessary changes during pregnancy, or they have insufficient tissue to begin with.
To boost milk supply, lactation consultants often recommend:
- Frequent feeding or pumping: Pumping for 10-15 minutes after feedings can help stimulate milk production.
- Skin-to-skin contact: This can encourage milk flow and help strengthen the bond between mother and baby.
- Hydration and nourishment: Staying hydrated and eating enough is necessary for maintaining a good milk supply.
While some women may struggle with a low supply, others may experience an overproduction of milk. Each case is unique, so seeking help from a lactation consultant can be incredibly beneficial. Some herbal supplements like fenugreek, goat’s rue, and chasteberry are thought to help boost milk supply, though more research is needed to confirm their effectiveness.
Final Thoughts
Pregnancy and lactation bring unique challenges for women with PCOS, but with the right support and dietary management, they can successfully navigate these stages. Balanced nutrition, physical activity, and open communication with healthcare providers are key to promoting a healthy pregnancy and successful breastfeeding journey. Whether it’s managing gestational diabetes risk or boosting milk supply, dietitians can play an invaluable role in guiding women with PCOS toward a healthy, fulfilling pregnancy and beyond.
Remember, every woman’s experience with PCOS is different, so it’s important to personalize your approach and seek out the resources that work best for you.
If you’re navigating pregnancy or breastfeeding with PCOS and need personalized guidance, don’t hesitate to reach out! Whether you have questions about nutrition, supplements, or managing PCOS symptoms, we’re here to support you on your journey to a healthy and happy pregnancy. Contact us today to schedule a consultation and take the next step toward a balanced, confident pregnancy experience!
References
Abdou, R. M., & Fathey, M. (2018). Evaluation of early postpartum fenugreek supplementation on expressed breast milk volume and prolactin levels variation. Egyptian Pediatric Association Gazette, 66(3), 57–60. https://doi.org/10.1016/j.epag.2018.07.003
Amin, A. F., Shaaban, O. M., & Bediawy, M. A. (2008). N-acetyl cysteine for treatment of recurrent unexplained pregnancy loss. Reproductive BioMedicine Online, 17(5), 722–726. https://doi.org/10.1016/s1472-6483(10)60322-7
Brand, K. M. G., Saarelainen, L., Sonajalg, J., Boutmy, E., Foch, C., Vääräsmäki, M., Morin-Papunen, L., Schlachter, J., Hakkarainen, K. M., & Korhonen, P. (2022). Metformin in pregnancy and risk of adverse long-term outcomes: a register-based cohort study. BMJ Open Diabetes Research & Care, 10(1), e002363. https://doi.org/10.1136/bmjdrc-2021-002363
Chaste tree. (n.d.). Stanford Medicine Children’s Health. https://www.stanfordchildrens.org/en/topic/default?id=chaste-tree-19-ChasteTree
Davidson, K. W., Barry, M. J., Mangione, C. M., Cabana, M., Caughey, A. B., Davis, E. M., Donahue, K. E., Doubeni, C. A., Kubik, M., Li, L., Ogedegbe, G., Pbert, L., Silverstein, M., Stevermer, J., Tseng, C., & Wong, J. B. (2021). Screening for gestational diabetes. JAMA, 326(6), 531. https://doi.org/10.1001/jama.2021.11922
DiNicolantonio, J. J., & O’Keefe, J. H. (2022). Myo-inositol for insulin resistance, metabolic syndrome, polycystic ovary syndrome and gestational diabetes. Open Heart, 9(1), e001989. https://doi.org/10.1136/openhrt-2022-001989
Engeroff, T., Groneberg, D. A., & Wilke, J. (2023). After Dinner Rest a While, After Supper Walk a Mile? A Systematic Review with Meta-analysis on the Acute Postprandial Glycemic Response to Exercise Before and After Meal Ingestion in Healthy Subjects and Patients with Impaired Glucose Tolerance. Sports Medicine, 53(4), 849–869. https://doi.org/10.1007/s40279-022-01808-7
Ershad, M., Naji, A., Patel, P., & Vearrier, D. (2024, February 29). N-Acetylcysteine. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537183/
Increasing milk supply – La Leche League USA. (2022, May 20). La Leche League USA. https://lllusa.org/increasing-milk-supply/
Mostajeran, F., Tehrani, H. G., & Rahbary, B. (2018). N-Acetylcysteine as an Adjuvant to Letrozole for Induction of Ovulation in Infertile Patients with Polycystic Ovary Syndrome. Advanced Biomedical Research, 7(1), 100. https://doi.org/10.4103/abr.abr_157_17
Motuhifonua, S. K., Lin, L., Alsweiler, J., Crawford, T. J., & Crowther, C. A. (2023). Antenatal dietary supplementation with myo-inositol for preventing gestational diabetes. Cochrane Library, 2023(2). https://doi.org/10.1002/14651858.cd011507.pub3
Mustaniemi, S., Vääräsmäki, M., Eriksson, J. G., Gissler, M., Laivuori, H., Ijäs, H., Bloigu, A., Kajantie, E., & Morin-Papunen, L. (2018). Polycystic ovary syndrome and risk factors for gestational diabetes. Endocrine Connections, 7(7), 859–869. https://doi.org/10.1530/ec-18-0076
National Institute of Child Health and Human Development. (2024, August 15). Goat’s Rue. Drugs and Lactation Database (LactMed®) – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK501817/
Polycystic ovary syndrome | Office on Women’s Health. (n.d.). OASH | Office on Women’s Health. https://www.womenshealth.gov/a-z-topics/polycystic-ovary-syndrome
Szczuko, M., Kikut, J., Szczuko, U., Szydłowska, I., Nawrocka-Rutkowska, J., Ziętek, M., Verbanac, D., & Saso, L. (2021). Nutrition Strategy and Life Style in Polycystic Ovary Syndrome—Narrative Review. Nutrients, 13(7), 2452. https://doi.org/10.3390/nu13072452